
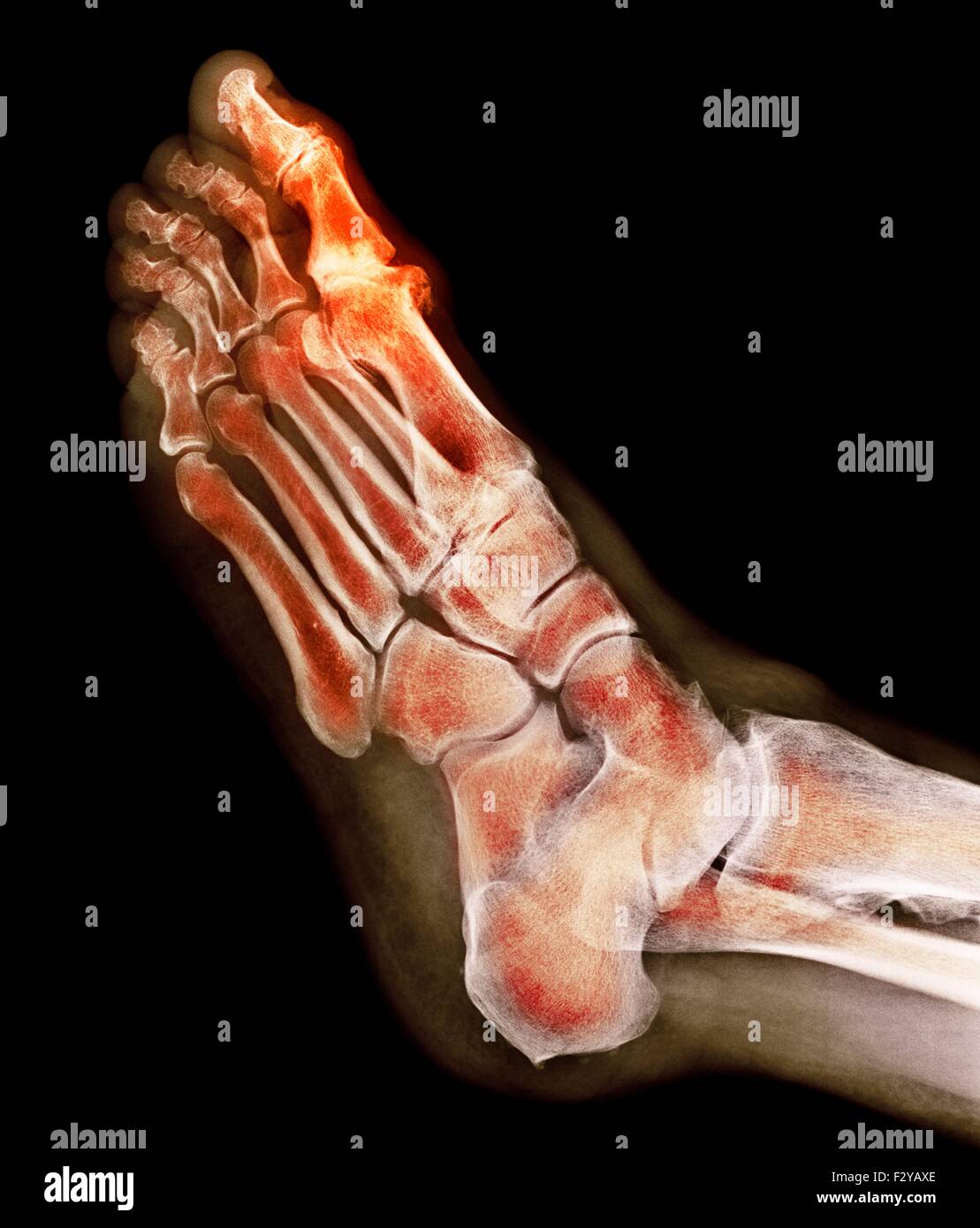
22 – 24 A further shortcoming has been said to be inconsistent interpretation and application of the grades between studies. 20, 21 While a generic system such as K&L has the advantage of allowing prevalence and features of OA at different sites to be compared, it has been criticized for relying heavily on the presence of osteophyte and for grading features of OA in such a way that assumes osteophyte formation chronologically precedes joint space narrowing and subchondral sclerosis in the pathogenesis of OA. The majority (90%) of studies included in the recent systematic review used the K&L grading system which is widely used to grade radiographic OA at a range of different joint sites. 19Ī significant barrier to the study of foot OA has been the lack of a foot-specific grading system to define radiographic foot OA. 15, 17, 18 One in 10 people aged over 70 years will develop new disabling foot pain over a 3-year period. Foot pain affects one in four people aged over 75 years, two-thirds of whom have related locomotor disability. 13 – 16 The prevalence and incidence of foot pain and related disability increase with age. OA seems likely to be a significant cause of foot pain in older people, in whom painful foot disorders are major contributors to restricted activity, locomotor disability, poor balance and risk of falling, and account for a substantial number of healthcare consultations.
#Mtp foot trial#
11 A Cochrane review published in 2010 included only one randomized trial of interventions for first metatarsophalangeal (MTP) joint OA.
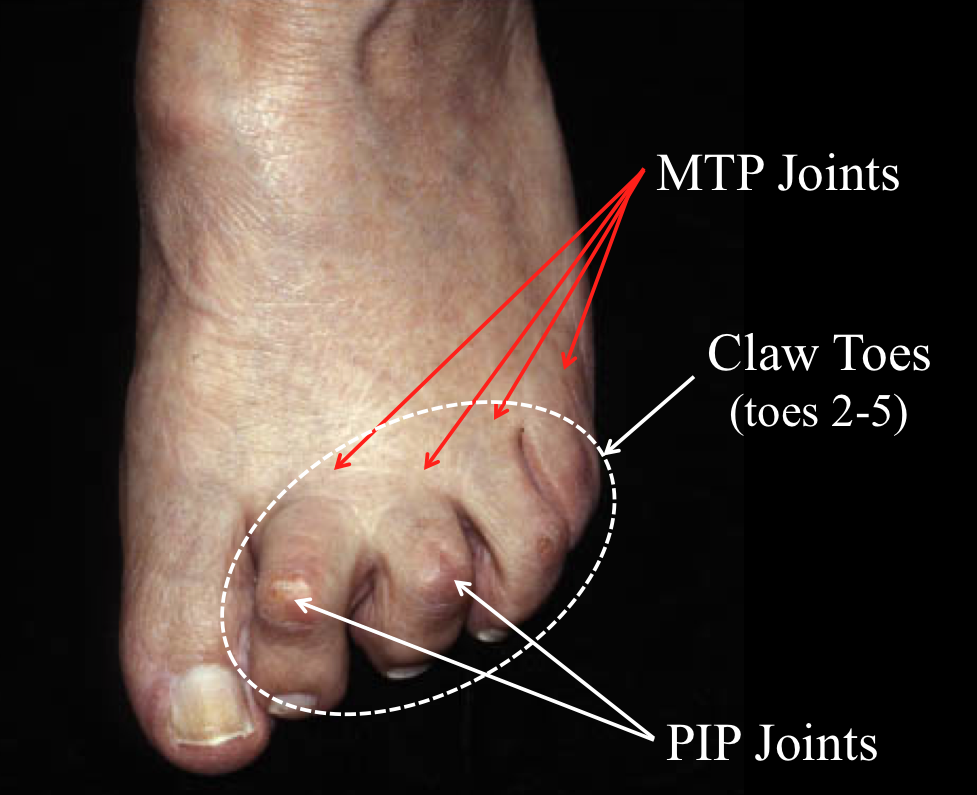
9 This contrasts greatly with the findings of similar reviews published 2 years earlier which identified 176 population-based epidemiological studies of radiographic hand OA 10 and 190 studies that had applied the Kellgren and Lawrence (K&L) grading system to knee OA. A systematic review of population-based epidemiological studies of radiographic foot OA published in 2010 identified only 27 publications arising from 22 studies. 7 The foot was included in early descriptions of generalized OA, 8 yet most subsequent OA research has focused on the knee, hip and hand. 3 OA leads to significant impairments of quality of life, 4 locomotor function, 5 social participation 6 and economic productivity. 1, 2 Musculoskeletal problems are the commonest reason for consultation in primary care, and OA accounts for 15% of these in people aged 45 years and over. Symptomatic osteoarthritis (OA) affects 10% of people aged over 60 years and is the leading global cause of years lost to disability in older people. Prospective epidemiological studies and randomized trials are needed to establish the incidence, progression and prognosis of foot OA and determine the effectiveness of both commonly used and more novel interventions. Existing trials provide some evidence of the effectiveness for pain relief of physical therapy, rocker-sole shoes, foot orthoses and surgical interventions in first metatarsophalangeal joint OA and prefabricated orthoses in midfoot OA. There are few randomized controlled trials in foot OA. Epidemiological studies suggest the existence of distinct first metatarsophalangeal joint and polyarticular phenotypes, which have differing clinical and risk factor profiles. The first metatarsophalangeal joint is most commonly affected, followed by the second cuneometatarsal and talonavicular joints. Symptomatic radiographic foot OA affects 17% of adults aged 50 years and over. Most existing studies focus on the first metatarsophalangeal joint, with evidence relating to midfoot OA being particularly sparse. Foot osteoarthritis (OA) is a common problem in older adults yet is under-researched compared to knee or hand OA.


 0 kommentar(er)
0 kommentar(er)
